
Electrocardiogram (EKG): Electrical pulses generated by your heart are measured and evaluated to determine if any cardiac problems exist.Blood tests: Blood tests can determine if you have developed any other conditions that may affect your heart’s performance.The following diagnostic procedures may be used to identify heart failure. Speak with your primary care doctor about signs of heart failure, or make an appointment with a heart and vascular expert at Bayhealth. Heart failure may present all of these symptoms or none of them. Physical weakness: A decrease in heart function can cause less blood to reach vital organs and muscles, resulting in physical weakness, fatigue, dizziness, or confusion.This may result in an irregular or rapid heartbeat. Heartbeat irregularities: A weakened heart may beat faster to ensure enough blood circulates through the body.Fluid retention and swelling: Heart failure can cause less blood to reach your kidneys, which can lead to fluid retention around your legs, ankles, and abdomen.Congestion: When the heart functions less efficiently, it can cause fluid to build up in the lungs, which can lead to wheezing, coughing, or shortness or breath.Depending on the cause and severity of your condition, symptoms may include the following. Signs of heart failure may develop suddenly or gradually over time. The following conditions may contribute to heart failure. are living with some form of heart failure, according to data from the Centers for Disease Control and Prevention (CDC). Though the condition does not mean your heart has stopped working, it can lead to serious health complications. doi:10.1161/ failure, also called congestive heart failure, occurs when the muscles of the heart become weakened and start to pump blood less efficiently. Rapid and Highly Accurate Prediction of Poor Loop Diuretic Natriuretic Response in Patients With Heart Failure. Testani JM, Hanberg JS, Cheng S, et al.World Health Organization International Agency for Research on Cancer 2018 () (estimated number of new breast and ovarian cases in 2018 (crude rate)).
EASL clinical practice guideliones on the management of ascites, spontane bacterial peritonitis, and hepatorenal syndrome in cirrhosis. European Association for the Study of the Liver.(2004) (stating refractory ascites occurs in 5 to 10 percent of patients with ascites) GlobalData NASH Epidemiology Forecast to 2026.

Centers for Disease Control and Prevention, Health, United States 2016, Chartbook on Long-term trends in Health, Table 20 () A concentration that is too high will result in hypernatremia and a concentration that is too low will result in hyponatremia. Maintaining a constant concentration of sodium in the body is a key physiological parameter that is vital to patient health. Once patients become resistant or intolerant to diuretics or begin to experience kidney failure, clinical alternatives are limited and have significant limitations. Sourceįluid overload is currently treated through the administration of diuretics, which frequently cause patients to develop kidney failure and an estimated 40% of heart failure patients experience diuretic resistance or intolerance. The cost of heart failure-related hospitalisations in the U.S. In addition, 1 in 4 patients are readmitted within 30 days, and 1 in 2 patients are readmitted within 6 months from discharge. admitted annually to hospital for heart failure, and 90% of these admissions are due to symptoms of fluid overload. There are approximately 1 million people in the U.S.
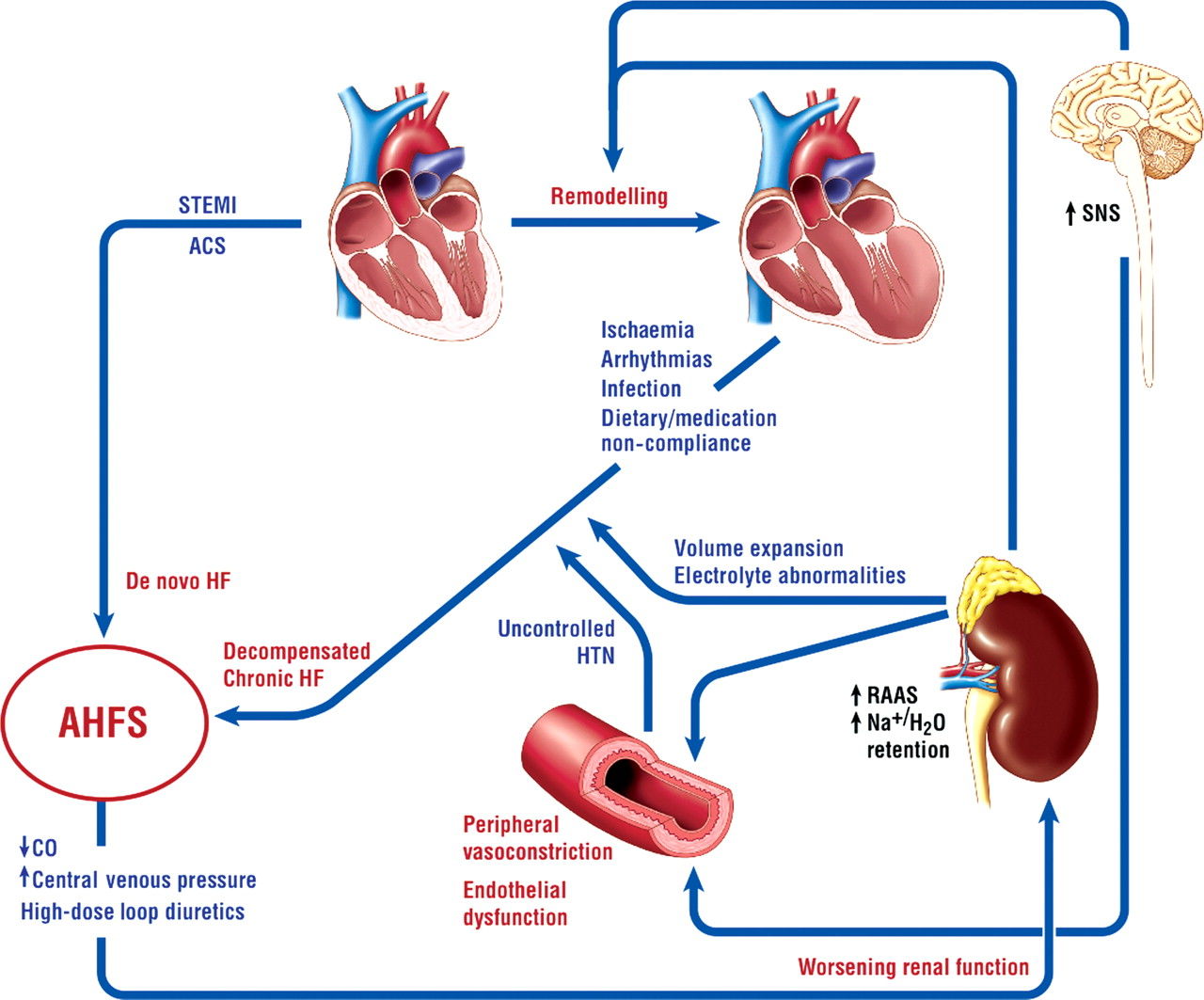
Fluid overload is a major clinical problem and the leading cause of hospitalisations for patients suffering from heart failure.


 0 kommentar(er)
0 kommentar(er)
